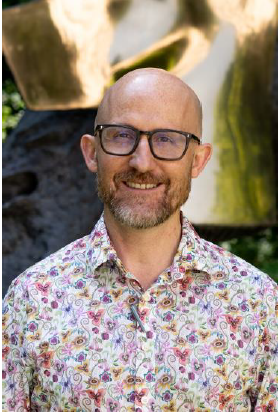
LGBT+ History Month: Q&A with Dr. Tristan Barber

Dr Tristan Barber is an HIV and Sexual Health Consultant at the Ian Charleson Day Centre, Royal Free Hospital, and Honorary Associate Professor at the Institute for Global Health at UCL. He has been living with HIV for over 20 years. He has a research background in HIV-related neurocognitive impairment and established a dedicated frailty and complexity service for people living with HIV (Sage Clinic). Tristan is currently Honorary Secretary for BHIVA, as well as Chair of the BHIVA Education and Scientific Subcommittee, Chair of the EACS Young Investigator Network, and Chair of the Board of Trustees for Positively UK. He is a member of National AIDS Trust’s Clinical Advisory Group.
Can you tell me a bit about your work with National AIDS Trust?
The initial campaign I worked with NAT closely on was changing a Private Members Bill that was going through Parliament about biting and spitting incidents with emergency service workers, where there was an attempt to include mandatory HIV testing for assailants even when the risk of transmission was zero. It was really exciting to use science and evidence to change something that was potentially going to cause more harm than good.
And for nearly five years now, we’ve been working on trying to change the regulations and law around sperm and egg donation for people living with HIV - because we know that people can do this safely. In the last six months, we’ve had confirmation from the Government that they will enact a change in the law to allow people with HIV, who had previously been prohibited from doing so, to donate their sperm and eggs to other partners.
I think being involved in these change processes with so much passion from everyone is a real buzz and part of my job that I really, really enjoy.
The theme for LGBT+ History Month this year is Medicine: #UnderTheScope, and celebrates and remembers the contributions of LGBT+ people in the fields of medicine and healthcare. Can you tell me a bit about what this theme means to you?
I think like many groups in medicine who've not previously held the spotlight, LGBT+ people have historically contributed a huge amount to healthcare. Historically LGBT+ people gravitated towards certain specialties where they felt they would be accepted. With the HIV epidemic, we did see a dramatic influx in terms of LGBT+ people becoming part of virology and sexual health specialties to help and support people who were affected by HIV. I think we historically gravitated towards those specialties where we felt comfortable, where we felt we had a home, we're accepted and where we could be ourselves.
We really need to celebrate the progress that's been made on an individual level, in terms of people feeling personally accepted, but also people in medicine becoming more diverse and more tolerant. LGBT+ History Month remains a very important month and a very important time to put LGBT+ people in healthcare under the spotlight.
Why do you feel that it is important for clinicians and charities like ourselves to work collaboratively in the interest of LGBT+ people?
I think the benefits of clinicians working with an organisation like National AIDS Trust and with LGBT+ people are that we understand how attitudes to healthcare and to being LGBT+ have diversified.
We still see people who are marginalised because of their sexuality. I think it's wrong that we assume all the barriers have been broken down just because we have access to marriage, because we have access to adopting children, because we're very unrestricted in terms of the careers that we can apply for. We also need to remember that not everyone with diverse sexuality will fit into the model of gay marriage or gay parenting, which may be seen as very heteronormative ideals for some.
I'll be 50 next year and the way I think about my own sexuality, my own healthcare perhaps is very different to an 18-year-old who identifies as LGBT+. I think we need to understand what it means across the lifecourse so we understand newer issues that we need to continue to advocate for and challenge.
Certainly in my work with NAT in recent years we've seen issues coming up around people with HIV who want to take up boxing or people who want to be in the armed forces whilst taking PrEP that have been restricted. Communities continue to experience stigma in different ways and people are now reaching new boundaries. By connecting with them and working collaboratively we can find the next barrier that we need to knock down.
How would you encourage people to get involved and celebrate LGBT+ History Month?
I think the important thing for people to do to celebrate LGBT+ History Month is to look at what's going on in their local environment and to look at the things that they've been involved with or affected by. For example, I have a patient in his 70’s who recently was asked to raise the Pride flag at his local hospital as recognition of his involvement in the voluntary sector, working with people with HIV and people who are LGBT+ over the last two decades. I think that was a fantastic tribute to him that he was asked to do that at his local hospital.
In the future, what things do you think still need to happen to improve LGBT+ inclusion in healthcare, both for staff and patients?
It remains the fact that there is a postcode lottery in terms of your ability to access LGBT+ inclusive services. I think we need to remove barriers to accessing care. We're going to see the need for diverse services across the life course. Having lost many people during the AIDS pandemic in the 80’s and 90’s, we are now starting to see an increase in the number of older LGBT+ people, with or without HIV, and these people are going to need inclusive elderly care services that understand their needs.
What we need to see is an increase in inclusive services that are not restricted to traditional ones that focus on LGBT+ people, and that are not restricted to gender, HIV and sexual health services. I think we now need a quality marking of other services to show their level of inclusivity and push for acceptance and services that are welcoming in all aspects of healthcare.
For staff, I think it’s clear from data that people in urban centres feel quite comfortable working in different specialities and being open about their sexual orientation - that’s not necessarily true across all parts of the UK. We must keep supporting staff that work in areas where inclusion is not as good as it should be. People need to see others with this lived experience of working in diverse specialities and keep pushing for change so that we see LGBT+ people working in all aspects of medicine - so that the community they represent can be provided for adequately and inclusively.